Items filtered by date: March 2022
How to Know if You Have an Ingrown Toenail
 You probably have an ingrown toenail (onychocryptosis) if the edge of your toenail grows into the skin of your toe. The area around the nail will likely be red and painful because it is irritated. If it progresses to infection, the skin might bulge around the nail and pus, or a clear fluid can be present. It stands to reason that the longer this condition is left untreated, the more likely it is to become infected. Ingrown toenails may be caused by wearing shoes that crowd the toenails, improper cutting of toenails, injury to the toenail, or toenails that are unusually curved. If you suspect you have an ingrown toenail or any other foot discomfort, you should visit a podiatrist for proper diagnosis and treatment.
You probably have an ingrown toenail (onychocryptosis) if the edge of your toenail grows into the skin of your toe. The area around the nail will likely be red and painful because it is irritated. If it progresses to infection, the skin might bulge around the nail and pus, or a clear fluid can be present. It stands to reason that the longer this condition is left untreated, the more likely it is to become infected. Ingrown toenails may be caused by wearing shoes that crowd the toenails, improper cutting of toenails, injury to the toenail, or toenails that are unusually curved. If you suspect you have an ingrown toenail or any other foot discomfort, you should visit a podiatrist for proper diagnosis and treatment.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Dr. Thomas E. Silver of Westwood Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenail Care
An ingrown toenail is a nail that has curved downward and grows into the skin. This typically occurs at the nail borders, or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. Milder cases that don’t involve infection or other medical conditions can benefit from soaking the feet in room-temperature water and gently massaging the side of the nail. In most cases, however, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Plantar Warts Can Be Treated!
Plantar Warts Can Be Treated!
What You Should Know if You Have Heel Pain
If you have heel pain, you may have come across the medical term plantar fascia. This is a strong, fairly inflexible connective tissue on the bottom of the foot that connects the heel bone with the toes. When this tissue becomes damaged or torn, it is known as plantar fasciitis, a painful inflammation of the plantar fascia. There is a good chance that your heel pain may be caused by plantar fasciitis, as this is the most common form of heel pain. What caused your plantar fasciitis? Perhaps you run or walk quite a bit or have the type of job that requires you to stand for all or most of the day. Maybe you regularly wear flip-flops, high heels or other footwear that does not offer adequate support or cushioning. Arthritis can contribute to the development of plantar fasciitis, as well as tight calf muscles, high arches, flat feet, or other conditions you may have that cause an imbalance in the biomechanics of your feet. You may even be pregnant or carrying some extra weight, which can stress the plantar fascia. Whatever the reason is for your heel pain, you should know that help is available. You don’t need to learn to live with heel pain, especially if it is caused by plantar fasciitis. Podiatrists treat people with plantar fasciitis every day, and can offer you various forms of treatment to provide the relief you are looking for.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Read more about Plantar FasciitisPlantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What You Should Know if You Have Heel Pain
If you have heel pain, you may have come across the medical term plantar fascia. This is a strong, fairly inflexible connective tissue on the bottom of the foot that connects the heel bone with the toes. When this tissue becomes damaged or torn, it is known as plantar fasciitis, a painful inflammation of the plantar fascia. There is a good chance that your heel pain may be caused by plantar fasciitis, as this is the most common form of heel pain. What caused your plantar fasciitis? Perhaps you run or walk quite a bit or have the type of job that requires you to stand for all or most of the day. Maybe you regularly wear flip-flops, high heels or other footwear that does not offer adequate support or cushioning. Arthritis can contribute to the development of plantar fasciitis, as well as tight calf muscles, high arches, flat feet, or other conditions you may have that cause an imbalance in the biomechanics of your feet. You may even be pregnant or carrying some extra weight, which can stress the plantar fascia. Whatever the reason is for your heel pain, you should know that help is available. You don’t need to learn to live with heel pain, especially if it is caused by plantar fasciitis. Podiatrists treat people with plantar fasciitis every day, and can offer you various forms of treatment to provide the relief you are looking for.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Signs of Peripheral Artery Disease
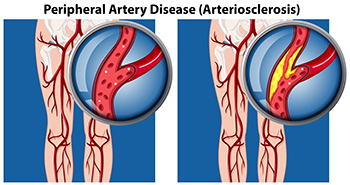 A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
A condition common among the diabetic community is peripheral artery disease, PAD, which affects between 8-10 million people a year in the United States. Many of them are over 50 years old, studies show. PAD causes fatty buildup in the arteries, including those in the feet. The clogged arteries restrict blood flow, and if left undetected can lead to severe tissue damage. Among the most common symptoms of PAD are pain and numbness, especially when walking. Weakness, cold feet, and wounds that take a long time to heal are also telltale signs to look out for. Taking proper medication to reduce the inflammation in the arteries is important, along with regular exercise, eating nutritious foods, and giving up smoking. In severe cases of PAD, medication and lifestyle changes may not be enough. If the condition persists, it is suggested that you make an appointment with a podiatrist as soon as possible for an evaluation and extensive treatment plan.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Thomas E. Silver from Westwood Foot Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Golden Valley, MN . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Read more about Peripheral Artery Disease